Get Healthy!
- Posted August 31, 2023
Gene-Tweaked Stem Cells Offer Hope Against Sickle Cell Disease
A type of gene therapy that precisely "edits" a key bit of DNA might offer a new way to treat sickle cell disease -- a painful inherited condition that largely strikes Black children and adults.
That's according to a new study in the New England Journal of Medicine describing the treatment -- a one-time but intensive process.
So far, researchers have tested it in only three young adults who were severely ill with sickle cell disease. But the early results are "promising," said study leader Dr. Akshay Sharma, of St. Jude Children's Research Hospital in Memphis, Tenn.
The patients saw reductions in pain attacks and other symptoms in the six to 18 months after receiving the gene therapy. One patient who had averaged one pain attack per month had none for nine months after the treatment.
"That's a huge improvement in quality of life," Sharma said.
The findings add to evidence that gene therapy can give sickle cell patients a path to a cure. Several gene therapy approaches are under development for the disease, and two have been submitted for approval to the U.S. Food and Drug Administration.
Sickle cell disease is an inherited disorder that mainly affects people of African, South American or Mediterranean descent. In the United States, about 1 in 365 Black children is born with the condition, according to the U.S. Centers for Disease Control and Prevention.
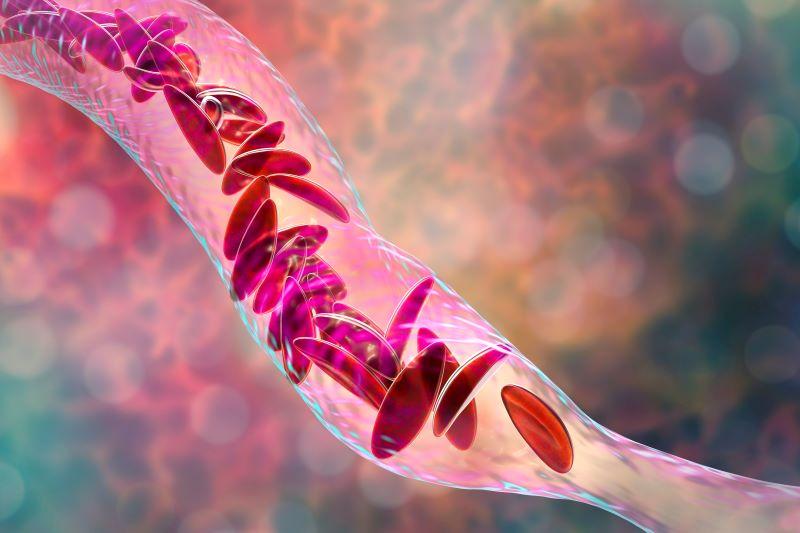
It arises when a person inherits two copies of an abnormal hemoglobin gene -- one from each parent. Hemoglobin is an oxygen-carrying protein in red blood cells.
When blood cells contain "sickle" hemoglobin, they become abnormally shaped and tend to be sticky. Those cells can block blood flow, causing serious pain "crises" and other symptoms. Over time, the disease can damage organs, sometimes leading to complications like strokes and heart disease.
There are medications for sickle cell disease that can ease pain and help prevent complications. But some patients do not fare well with drugs alone, Sharma said.
In those cases, there is one potential cure: a stem cell transplant. In that procedure, doctors use chemotherapy drugs to wipe out a patient's bone marrow stem cells, which are producing the faulty blood cells. Those cells are then replaced by stem cells from a healthy donor.
That's if they can find a donor, Sharma said. The ideal donor is a sibling who is genetically compatible and free of sickle cell disease -- an uncommon scenario.
"For those patients, I think gene therapy will be the only option going forward," Sharma said.
In general, gene therapies for sickle cell involve removing some of a patients' bone marrow stem cells, then sending them to a lab to be genetically tweaked. While that's happening, the patient undergoes chemo to kill off the remaining faulty stem cells, making room for an infusion of the genetically revamped cells.
In some approaches, the genetic tweaking is done by exposing stem cells to a virus that inserts a healthy copy of the flawed hemoglobin gene.
More recently, researchers have used CRISPR-Cas9, an editing tool that allows them to precisely "snip" bits of DNA within a cell, to make repairs or perform other alterations.
One of the gene therapies up for FDA review, called exa-cel, uses CRISPR-Cas9.
Sharma's team also used CRISPR. But the specific genetic target is novel, he explained: The researchers sought to re-create a natural phenomenon, in which some people have a benign genetic alteration that causes them to keep producing fetal hemoglobin instead of making the normal "switch" to adult hemoglobin.
In people with sickle cell, fetal hemoglobin can substitute for the faulty adult version.
For the three patients in the new study, the gene therapy did spur them to stably produce fetal hemoglobin. And over the next six to 18 months, each patient had one pain attack.
The big advantage of gene therapy over stem cell transplants is that it takes the donor out of the equation, according to Dr. David Williams, chief of hematology/oncology at Boston Children's Hospital.
That skirts the risks of transplants, such as rejection and a complication called graft-versus-host disease, said Williams, who is studying gene therapy for sickle cell.
That said, big questions still loom, according to Williams: To what degree can gene therapies reverse sickle cell complications? How long do the effects last? Will safety issues come up in the years after treatment?
There are also issues beyond what trials can show, Sharma pointed out. Science can prove that gene therapy works, he said, but how many patients will be eager to try it?
People can be understandably "skeptical" of a new medical therapy, Sharma said. Plus, gene therapy is no picnic: It still requires hospitalization for chemo, and the whole process, start to finish, takes about a year, Sharma said.
Then there's the question of who will pay.
"We don't know what these therapies will cost," Sharma said, "but it could be between $2 million and $3 million."
Whether insurers will foot that bill remains to be seen. A recent study estimated that the one-time cost of gene therapy would outweigh the lifetime cost of treatments that sickle cell patients now undergo -- including repeated blood transfusions and hospitalizations.
At the same time, Sharma said, if gene therapy can spare patients of those other treatments, it would be hard to put a price tag on their gains in quality of life.
The findings were published Aug. 31.
More information
The U.S. Centers for Disease Control and Prevention has more on sickle cell disease.
SOURCES: Akshay Sharma, MBBS, assistant member, faculty, bone marrow transplantation and cellular therapy, St. Jude Children's Research Hospital, Memphis, Tenn.; David Williams, MD, chief of hematology/oncology, Boston Children's Hospital, associate chairman, pediatric oncology, Dana-Farber Cancer Institute, Boston, and professor, pediatrics, Harvard Medical School, Boston; New England Journal of Medicine, Aug. 31, 2023
